Nine Things You May Be Surprised to Know About VNSNY’s HOPE Program
Since 2015, VNSNY Hospice’s HOPE (Hospice Outreach, Patient and Provider Education) Program has encouraged better access to hospice care among African Americans and Latinx in Harlem. Recently, thanks to a $500,000 grant from the Mother Cabrini Health Foundation, HOPE has expanded to the Bronx as well.
Here are nine things you may not know about the HOPE Program:
 1. The HOPE Program is a key part of VNSNY’s effort to address health disparities. Nationwide, 48% of white Medicare beneficiaries enroll in hospice, compared with 8% of Black and 6% of Latinx Medicare beneficiaries. This stark disparity means that millions of Americans are missing out on the many benefits of hospice care at the end of life, which includes getting skilled symptom management while living with their loved ones at home, rather than languishing in the hospital.
1. The HOPE Program is a key part of VNSNY’s effort to address health disparities. Nationwide, 48% of white Medicare beneficiaries enroll in hospice, compared with 8% of Black and 6% of Latinx Medicare beneficiaries. This stark disparity means that millions of Americans are missing out on the many benefits of hospice care at the end of life, which includes getting skilled symptom management while living with their loved ones at home, rather than languishing in the hospital.
 2. There are many reasons for the disparities in hospice use. They include lack of awareness or understanding of hospice and palliative care; lack of communication between health care providers and their patients about hospice; and misconceptions about hospice care—especially the idea that hospice care is inferior to hospital care. “The Bronx is a very important borough in terms of the impact we can have,” says Michelle Drayton, Director of Hospice and Palliative Outreach. “We want to help dispel misunderstandings about end-of-life care.”
2. There are many reasons for the disparities in hospice use. They include lack of awareness or understanding of hospice and palliative care; lack of communication between health care providers and their patients about hospice; and misconceptions about hospice care—especially the idea that hospice care is inferior to hospital care. “The Bronx is a very important borough in terms of the impact we can have,” says Michelle Drayton, Director of Hospice and Palliative Outreach. “We want to help dispel misunderstandings about end-of-life care.”
3. In the last 18 months the HOPE program has admitted 1,374 patients from Harlem and the Bronx. In addition to Michelle, the HOPE program consists of two Clinical Hospice Nurse Liaisons Ruthlyn Marrett and Clarissa Santos, both RNs. Many other staff members across VNSNY also help support the HOPE program, including Business Development and Community Mental Health Services. The HOPE program’s successful outreach activities have received extensive local media coverage in print and on radio and TV.
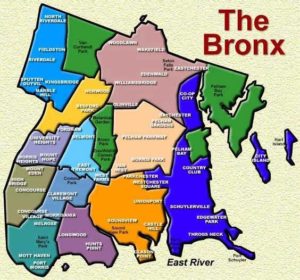
4. HOPE is concentrated on seven zip codes in Central Harlem. With its Bronx activities, the entire borough is included. In both boroughs, the focus is on the poorest neighborhoods, which tend to have the most significant disparities in health and outcomes.
 5. The HOPE Team expanded to the Bronx during the pandemic. “We never stopped with COVID-19,” says Michelle. “VNSNY Hospice and Palliative Care served almost 7,100 patients in 2020.” During this same time period, HOPE continued its extensive outreach in Harlem and launched its new program in the Bronx.
5. The HOPE Team expanded to the Bronx during the pandemic. “We never stopped with COVID-19,” says Michelle. “VNSNY Hospice and Palliative Care served almost 7,100 patients in 2020.” During this same time period, HOPE continued its extensive outreach in Harlem and launched its new program in the Bronx.
6. HOPE is working extensively with local hospitals and community organizations. Key hospital partners include Harlem Hospital and Jacobi, both a part of Health + Hospitals, and the Mount Sinai Health System. Community-based organizations are also important partners because they’re so trusted by the people they serve. “HOPE is far from a hospitals-only program,” Michelle notes. “We’re doing outreach and education efforts, talking to community leaders and communicating directly with patients in both hospitals and the neighborhoods.”
7. The HOPE program has hired a Faith Leader to work with religious leaders across the city about hospice care and end-of-life issues. Religious organizations are also important HOPE partners. Extensive VNSNY research, including a focus group with 15 Bronx faith leaders, showed that ministers, priests, and other faith leaders are important influencers when patients and their families are making end-of-life decisions.
 8. Here’s how a typical day for a Clinical Hospice Nurse Liaison such as Ruthlyn Marrett and Clarissa Santos starts: “Are you the lady that’s going to get me home?” Carlos (not his real name), a patient in Harlem Hospital, asked Ruthlyn. In the hours that followed, Ruthlyn did just that, helping Carlos to go home to Brooklyn after 65 days in two hospitals for treatment of COVID-19 and several chronic illnesses. She arranged for a hospital bed and other medical equipment to be installed in his residence, and built a VNSNY caregiving team that included a nurse, doctor, social worker, and spiritual care counselor to help his wife, Iris, and their family manage Carlos’s symptoms and navigate the emotional and logistical complexities of end-of-life care. “We’re here to educate. We show the family what to do and explain every step,” Ruthlyn says. “I told Iris she could call me anytime”—which she did. And Carlos? He was beyond thrilled to be home with his family.
8. Here’s how a typical day for a Clinical Hospice Nurse Liaison such as Ruthlyn Marrett and Clarissa Santos starts: “Are you the lady that’s going to get me home?” Carlos (not his real name), a patient in Harlem Hospital, asked Ruthlyn. In the hours that followed, Ruthlyn did just that, helping Carlos to go home to Brooklyn after 65 days in two hospitals for treatment of COVID-19 and several chronic illnesses. She arranged for a hospital bed and other medical equipment to be installed in his residence, and built a VNSNY caregiving team that included a nurse, doctor, social worker, and spiritual care counselor to help his wife, Iris, and their family manage Carlos’s symptoms and navigate the emotional and logistical complexities of end-of-life care. “We’re here to educate. We show the family what to do and explain every step,” Ruthlyn says. “I told Iris she could call me anytime”—which she did. And Carlos? He was beyond thrilled to be home with his family.
9. Having staff who understand the people of Harlem and the Bronx is critical. “Understanding people and their culture is how the HOPE program breaks down barriers and explains the benefits of hospice to both patients and families, while debunking the myths about what hospice is and isn’t,” says Michelle. “All of our hospice and related business staff have received cultural competence training, where they learn common perceptions and misperceptions about medical and hospice care as well as how to connect with different groups and different influencers such as family, friends, and ministers and priests.”
To read similar articles in the series on other teams in the organization, click here.


