Preventing Problems Before They Occur: How QAPI Helps Avoid Hospitalizations

When Iyabode “Yabo” Alfred recently reviewed the hospitalization rates for VNSNY’s home care patients, she noticed that the rates were especially high among those being treated for cancer. Looking more closely, she found that the reason for this didn’t have to do with their cancer directly, but rather to falls in the home related to the pain medications the patients were taking, which can impair a person’s sense of balance.
“Based on this discovery, we’re now focusing more intently on educating patients and their family caregivers about the need for safety precautions when taking these medications,” says Yabo. As Director of Quality Management Services for Home Care—a position she left recently to become an Assistant Professor of Nursing at Long Island University, though she also still serves as a per diem nurse in Central Intake—Yabo was responsible for implementing the new QAPI (Quality Assurance Performance Improvement) program from the Centers for Medicare and Medicaid Services (CMS).

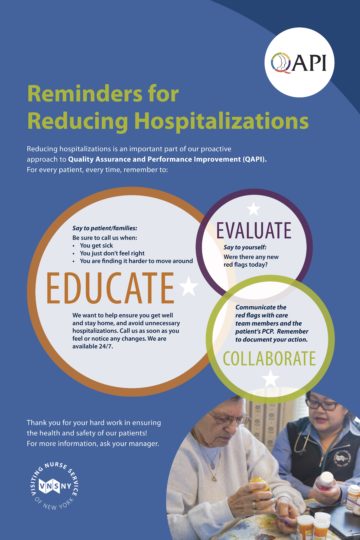
“QAPI is about getting in front of quality issues,” explains Angela Barody, Vice President of Quality and Customer Experience, who is overseeing the program. “Previously, something would happen and quality would get called in to do a retrospective review and try to fix the problem. With QAPI, everybody on the team is now more vigilant about making sure problems don’t occur in the first place.”
To develop its QAPI framework, VNSNY conducted an analysis of all the data in the agency’s outcome database to identify high-risk situations and began developing strategies to anticipate and prevent their occurrence. For example, a social worker might discover that a patient isn’t taking his meds because he can’t afford them. She’ll talk to his doctor who will then prescribe a less expensive drug, but until now there was only limited coordination regarding how this change was communicated to the patient’s field nurse. It’s an inadvertent problem caused by the compartmentalization of services—but now, with QAPI’s emphasis on team communication, these kinds of gaps won’t occur.
“We also found that nurses and therapists were sometimes differing in their functional assessments of patients, which can lead to reimbursement problems,” says Yabo. “So we’re now encouraging clinicians to communicate with each other around the assessment process.” Another oversight identified by Yabo and Peggy Taber, director of VNSNY’s Call Center, was the fact that not all the field clinicians were telling their patients about the call center, which functions like a patient hotline. When a patient isn’t feeling well and doesn’t have a home visit scheduled that day, he can phone the Call Center and a nurse will walk him through steps he can take to mitigate his symptoms, including anxiety—thereby avoiding the need for calls to 911 and potential trips to the ER. “By ensuring patients call VNSNY instead, our data shows that’s we’re almost always able to resolve clinical issues without sending the patient to the emergency department,” says Yabo.

The QAPI program is also reinforcing the importance of providing prompt, comprehensive education to patients and family members on how to self-manage of medical conditions. For VNSNY home care nurse Nancy Girlando, her QAPI training led her to redouble her education efforts with 82-year-old Sylvia, a heart failure patient who was recently discharged to her care. In addition to swollen legs and lack of energy, says Nancy, “Sylvia had a huge information deficit about her condition, despite being under a cardiologist’s care for years.”
Drawing on her QAPI training, Nancy swiftly took steps to bridge the gaps in Sylvia’s knowledge and self-care regimen and get the whole care team aligned with those goals. She brought Sylvia a copy of VNSNY’s patient manual on how to manage heart failure and reviewed it with her and her husband, highlighting relevant sections such as how to record her weight, blood pressure and oxygen levels every day. As Sylvia learned more about how to self-manage her heart failure, she dropped 10 pounds and felt more in control, confident, alert and happy. “She looked tremendously better after just six weeks,” says Nancy. “Now she’s going to her beach club and church again, and even attended a recent family wedding.”
“In the final analysis,” adds Angela, “QAPI is about improving outcomes, by providing a formal structure for how we provide services and care to our patients.”
Top 5 Things You Need to Know about QAPI
- QAPI (Quality Assurance Performance Improvement) is a CMS (Centers for Medicare and Medicaid Services) mandated program that all health care organizations are required to have in effect by January 2018.
- Pronounced “kwop-ee,” the new program targets gaps in knowledge or practice that are contributing to quality issues such as avoidable hospitalizations, falls, or infections, as well as problems that might arise around documentation.
- While VNSNY has always stressed patient education and careful management of medical conditions, QAPI takes this a step further, employing a proactive approach that aims to anticipate and address potential issues in patient care before they occur.
- Specific goals of the QAPI program include reduction of rehospitalizations and infections, timely initiation of care, effective pain management, and improvement of overall patient care and satisfaction.
- Starting last spring, an interdisciplinary review team has been providing feedback as the system was being rolled out. So far, the feedback has been consistently positive. “QAPI gives everyone a standardized process to follow,” says Angela Barody, Vice President for Quality and Patient Experience, “which is very helpful when people are trying to manage their busy days.” Knowing that everyone is following the same protocol also gives clinicians more confidence, she says.
The Take-Away: The new CMS-mandated QAPI (Quality Assurance Performance Improvement) program provides a standardized approach to identifying and addressing potential issues in coordination and delivery of patient care before they occur.

